

A Vascular Surgeon is a Board-Certified Physician who diagnoses and treats conditions in the arteries and veins of the circulatory system. These surgeons have completed General and Vascular Surgery training and manage all diseases affecting the vascular system, excluding the vessels of the heart and brain.
Most commonly, patients are referred to the Vascular Surgeon for care after seeing their Primary Care Doctor (Internal Medicine, Family Medicine, Pediatrics and OB/GYN), who is typically the first Specialist in their care to diagnose a condition which requires a vascular surgical intervention.
The level of expertise to surgically treat specific conditions and the credentials necessary are important factors when choosing the right physician. You may do your diligence and check the credentials and practice style of your doctor with the help of your family and friends. At myDoqter, we facilitate this process by providing you with access to patient feedback about doctors, as well as to the professional recommendations given by other physicians who have witnessed first-hand the expertise and professional competency of your Vascular Surgeon.
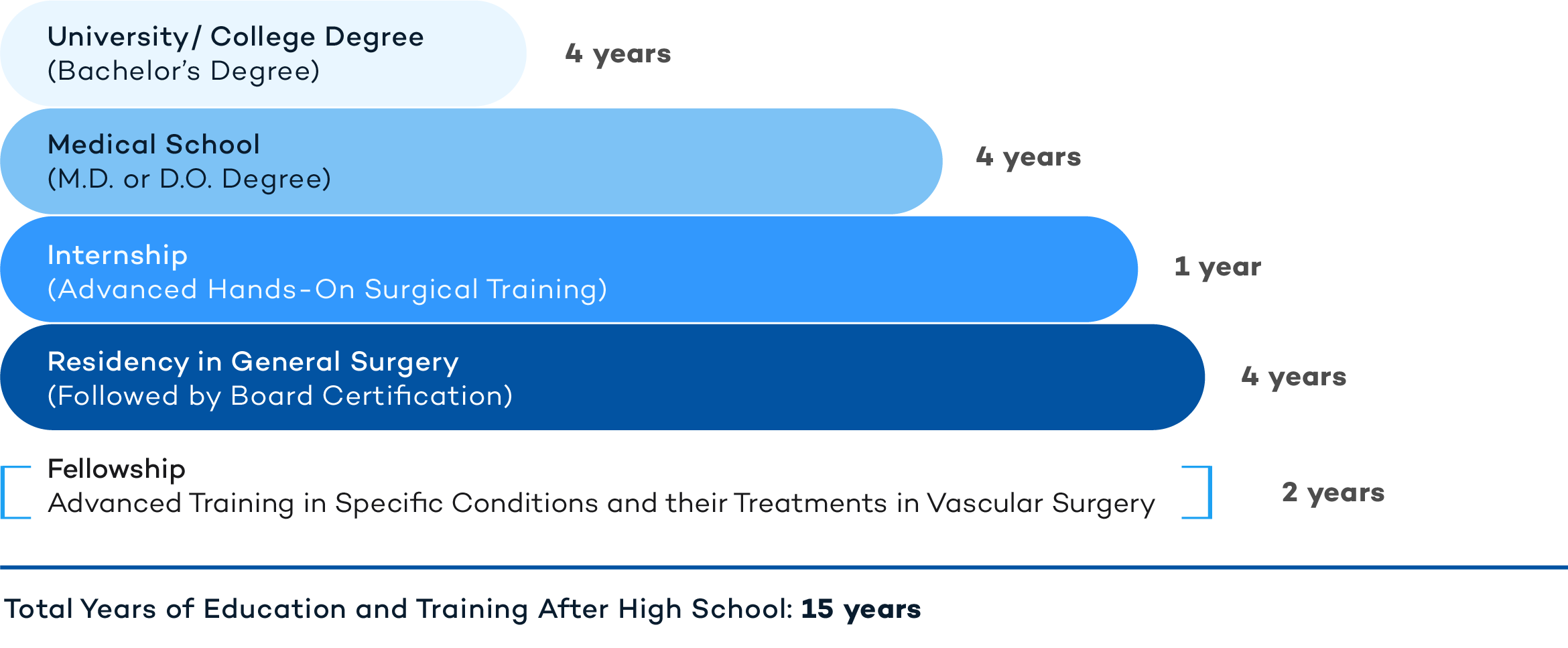
Vascular Surgeons are doctors (M.D. or D.O.) with advanced medical degrees and training. The typical route of training for a Vascular Surgeon involves the completion of a full General Surgical Residency, followed by a two-year fellowship in Vascular Surgery. The following is a representation of the years of education and training that vascular surgeons have undergone.
A Vascular Surgeon serves a critical role in the management of disease states of the vascular system that require surgical intervention. Some of the more common conditions they treat and procedures they perform include:
Aneurysm: An aneurysm is a localized weak spot on a blood vessel wall that causes the wall to bulge or balloon out and possibly rupture. Aneurysms are typically harmless and don’t show any symptoms unless they enlarge and/or rupture, at which point they may become life threatening. Aneurysms are classified based on their location in the body, with the brain and the heart most commonly affected. There are aortic aneurysms, cerebral aneurysms, and peripheral aneurysms. Aortic aneurysms occur when the wall of the aorta bulges beyond its normal 2-3cm diameter. The aorta may distend anywhere from its origin at the left ventricle of the heart, through the chest cavity, and into the abdomen. Abdominal aortic aneurysms are the most common of this type and may be deadly if left without surgical intervention. Cerebral aneurysms occur in the arteries that feed blood to the brain and may be life threatening if they rupture, leading to a type of brain bleed known as subarachnoid hemorrhage. Peripheral aneurysms may occur in other vessels in the body such as the popliteal artery, the splenic artery, the mesenteric artery, femoral artery, or the carotid artery in the neck. Not all aneurysms need treatment. If a rupture is suspected or anticipated, however, traditional open surgery or an endovascular surgical procedure may be performed. Endovascular surgery is a less invasive method of treating aneurysms whereby a stent graft is placed through small incisions to repair and essentially replace the vessel wall. Risk factors for aneurysms include hypertension, smoking, obesity and a poor diet.
Atherosclerosis: This term refers to the hardening and narrowing of arteries in the body. Atherosclerosis involves the buildup of plaques made of cholesterol deposits, calcium and fat, that can narrow and eventually block the arteries leading to heart attacks, stroke, peripheral arterial disease, and even death. Atherosclerosis can affect any artery in the body - the most common include Coronary Heart Disease, Carotid Artery Disease, Peripheral Artery Disease, and Chronic Kidney Disease. Atherosclerosis-associated events are the leading cause of death in the U.S. in both men and women. Poor lifestyle choices such as smoking, obesity, alcohol abuse, remaining sedentary, and poor eating habits contribute significantly to this disease state. Other health conditions like insulin-resistance, diabetes, hypercholesterolemia or sleep apnea may also contribute to the formation of plaques within the arteries. Vascular Surgeons will be the primary physician for Peripheral Vascular Diseases, but Coronary Artery Disease will require Cardiologists and possibly Cardiothoracic Surgeons to be involved, as well as Nephrologists in the case of Chronic Renal Disease.
Carotid Artery Disease (CAD): The carotid arteries in the neck supply oxygen to the brain. A stroke or mini stroke (Transient Ischemic Attack, or TIA) may occur when there is a narrowing or blockage of one of these arteries, and small plaques break off and travel to the brain. Symptoms of stroke due to CAD include: weakness, paralysis, confusion, difficulty speaking, loss of balance and difficulty walking, sudden and severe headaches, visual disturbances, and loss of consciousness. For many individuals with Carotid Artery Disease, there are no symptoms until they have the stroke or mini stroke. Diagnosis may be made with a stethoscope if a whistling sound (a bruit) is heard over the carotid artery on the neck. Otherwise the most common way to diagnose CAD is through a carotid duplex ultrasound. A CT scan, MRI, or angiogram can also be used to diagnose vessel narrowing and the extent of disease. Treatment for CAD is aimed at reducing the risk of stroke. Medications to lower cholesterol, blood pressure, and aspirin-based pills can help reduce stress on vessel walls, thereby reducing the risk of stroke. If vessel wall narrowing is more than 60%, then a surgical procedure may be recommended. Carotid endarterectomy (with vessel incision and physical plaque removal), or angioplasty (balloon insertion) or vessel stenting may be performed.
Deep Vein Thrombosis (DVT): This term refers to the formation of a clot in a vein deep in the body due to blood thickening and/or reduced blood flow. Most of these DVTs are in the legs, and the biggest concern is that these clots can break off and travel to other parts of the body as an embolus and cause tissue damage. Risk factors for DVT include obesity, smoking, certain inherited blood disorders (Factor V Leiden), taking certain medications such as oral contraceptive pills or hormone therapy, serious injuries such as broken bones or recent surgery, pregnancy and during the immediate postpartum period, underlying cancer, advanced age, and prolonged immobility. Diagnosis of a DVT may be made with a proper history and physical exam, where there is redness, swelling and tenderness of the leg or arm. An ultrasound, CT scan, or MRI may also be used to diagnose a DVT. A protein fragment released from the breakdown of a clot, called the D-dimer, can also be measured quantitatively and used to aid in diagnosis. Treatment of DVT is aimed at breaking down the clot, not allowing new clots to form, and preventing the clot from breaking off and causing further tissue damage. Anticoagulant medications (blood thinners) such as Warfarin and Heparin are used most commonly to break down these clots and may be required longtime to prevent new clot formation.
Pulmonary Embolism (PE): A Pulmonary Embolism occurs when one of these deep thromboses in the legs breaks off and travels to the arteries in the lungs and compromises blood flow. Symptoms of a PE include shortness of breath, coughing up blood, anxiety and restlessness, heart palpitations, sweating, hypotension, along with symptoms of a DVT (swelling, redness, warmth in an arm or leg). PE may be a difficult diagnosis to make and chest X-ray, CT scan, D-dimer, ventilation-perfusion (VQ) scan, Duplex ultrasound, or pulmonary angiogram may be used to help. Treatment for a PE depends on the severity of the disease and includes anticoagulant therapy (Warfarin and Heparin), a thrombolytic medication injected to dissolve a clot, pulmonary embolectomy (surgical removal of a clot), and placement of an Inferior Vena Cava (IVC) filter. An IVC filter is placed in the Inferior Vena Cava to essentially trap emboli (traveling fragments of clots) from the legs and prevent them from damaging the lungs.
Pelvic Congestion Syndrome (PCS): This syndrome is a common cause of chronic pelvic pain and involves the development of varicose veins in the pelvis below the abdomen in women. Blood then pools in these enlarged veins and causes pressure and pain in the groin. Diagnosis of PCS is made via Pelvic Venography, where a contrast dye is injected into the veins of the pelvis and then read via X-Ray. Treatment of PCS is through Pelvic Vein Embolization with internal plugging of the affected vessels.
Stroke: A stroke occurs when there is a sudden interruption of the blood supply to a portion of the brain. This blockage prevents oxygen and nutrients from reaching the brain tissue and cell death may begin within minutes. Strokes are true medical emergencies, and early intervention may reduce morbidity and be life-saving. There are two types of strokes: ischemic (blood vessels are blocked or narrowed) and hemorrhagic (a blood vessel in the brain ruptures or leaks). Signs of a stroke include: difficulty speaking or standing, paralysis, visual disturbances, headache, or difficulty walking. Suspected strokes will require a physical and neurologic exam, bloodwork, and imaging studies such as a CT scan, MRI, carotid ultrasound or echocardiogram. Initial treatment of a stroke is aimed at the underlying cause. Ischemic strokes require clot busting medications or direct endovascular procedures to remove the blockade. A hemorrhagic stroke requires reducing pressure in the brain and stopping the bleeding via surgical intervention or endovascular embolization (surgically filling the holes of the affected vascular tissue).
Varicose Veins: These enlarged veins occur in the legs and become swollen, twisted and bumpy due to faulty valves in the veins, which allows blood to pool causing further vessel distention. Advanced age, pregnancy, family history of varicosities, lower limb injuries, and weight gain all predispose to varicose vein development. Treatments for varicose veins include Sclerotherapy, Radiofrequency or Laser Ablation, and Phlebectomy. Sclerotherapy involves injecting a chemical irritant or “sclerosant” solution directly into the veins to cause localized clot formation, with eventual scar development and vessel collapse. Multiple treatments are typically required for Sclerotherapy to successfully collapse a varicose vein, but it is usually an easier, minimally invasive outpatient procedure. Endovenous thermal ablation with lasers or radiofrequency devices uses a thin catheter inserted into a vein to permanently seal it off with high energy heat. This procedure scars the treated veins and the body naturally resorbs them over time. This is also an outpatient procedure with minimal recovery time. Phlebectomy is surgical vein removal through tiny excisions in the leg. Phlebectomy is often performed after an ablation procedure to remove any residual veins that are too large for the body to resorb on its own.
Venous Ulcers: These ulcers appear on the legs as open sores due to long-standing venous hypertension and malfunctioning venous valves. These increased pressures in the blood vessels of the skin, and the presence of faulty valves, cause blood to pool in the lower extremities and leads to skin breakdown. Venous ulcers are painful and notoriously difficult to treat. Treatment in early stage disease is aimed at prevention of ulcers and reducing venous pressures in the lower legs through compression. Wrapping the legs with compression bandages is used in order to reduce the venous pressures upon standing. Daily compression bandages may also be used as a means for preventing venous insufficiency over time. Unna Boots can be applied to an affected leg by a Vascular Surgeon to further reduce venous pressures. Unna Boots involve moist gauze bandages that are applied and allowed to harden into a boot and are left in place for one to two weeks to allow more advanced Venous Ulcers to heal. Surgical management of Venous Ulcers may be indicated at any stage of disease. Tissue debridement to promote wound healing and the surgical interruption of influx are the mainstays of treatment.
Vascular Surgeons provide comprehensive surgical guidance for patients with a wide variety of vascular medical conditions. They are well versed in the anatomy and physiology of the human body and receive highly specific training to properly address illnesses and injuries that can be treated or cured through surgical interventions.
You can read more about Vascular Surgery in the following links:
https://vascular.org
https://scvs.org
https://vesurgery.org
https://www.jvascsurg.or