

A physician who specializes in Sports Medicine focuses primarily on the prevention and treatment of injuries resulting from any kind of athletic activity. Sports Medicine is not an individual specialty in itself so these physicians have their board certification in a variety of related medical specialties, including: Internal Medicine, Family Medicine, Emergency Medicine, Pediatrics, or Physical Medicine and Rehabilitation. A Sports Doctor specializes in the non-operative treatment of musculoskeletal conditions. These physicians treat adults and children, professional athletes, and those with injuries related to regular exercise or due to physically demanding occupations.
Sports Medicine Physicians manage a team of professionals to best address the needs of the injured athlete. Other members of the Sports Medicine team may include physical therapists, athletic trainers, massage therapists or dietitians. Each member of this team works together to address the underlying injury and to outline an appropriate treatment protocol to promote healing and a return to regular activities as soon as possible. Sports doctors also help manage acute or chronic illnesses, as well as nutritional needs or performance issues for athletes of all levels.
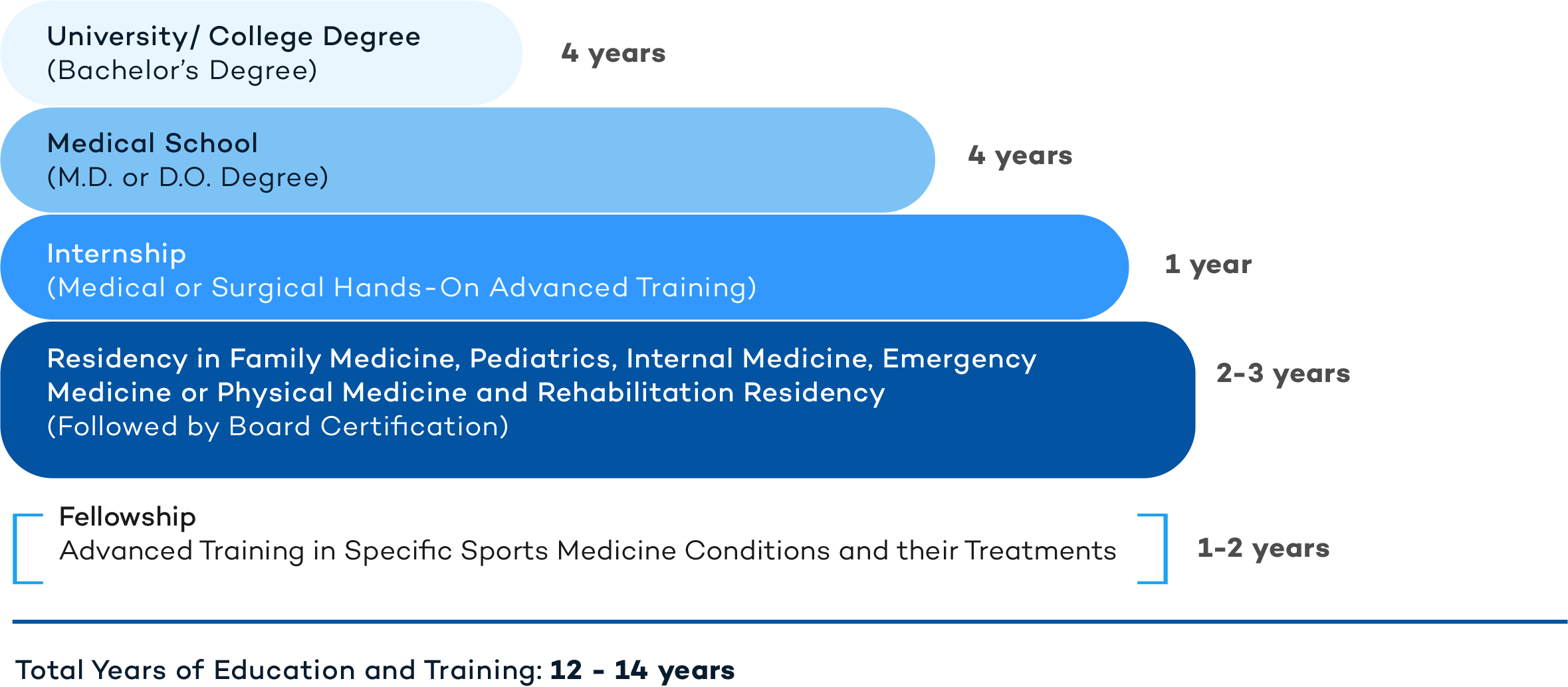
Sports Medicine specialists are doctors (M.D. or D.O.) with advanced medical degrees and training. The following is a representation of the years of education and training that a Sports Medicine Physician has undergone.
A Sports Medicine Physician will treat an extensive list of conditions associated with any sports-related or exercise-related injuries, including:
Sprains and Strains: These are common injuries for anyone participating in a sport or a repetitive exercise activity. A sprain is an injury (stretch or tear) of a ligament, the fibrous tissue that connects two bones in your joints. The ankle is one of the most common locations for a sprain, especially in athletes. Symptoms of a sprain may include pain, swelling and bruising. A strain, by contrast, is a stretch or tear of a muscle or tendon (the tissue that connects muscle to bones). Sprains and strains can usually be treated at home with rest, ice, compression, and elevation of the affected body part. Occasionally, physical therapy and/or surgery may be necessary for treatment if the sprain or strain fails to heal.
Fractures: Broken bones are called fractures. Traumatic injury, prolonged stress (overuse), or diseases that predispose to a reduced bone density (osteoporosis) are the most common causes of bone fractures. A bone may be partially or completely fractured, and may have a clean break or be broken in multiple pieces. Fracture severity is usually dependent upon the initial force that caused the break. Swelling, bone deformity and pain with bruising are the most common signs of a break. Treatment for bone fractures may involve cast immobilization, a functional cast, or surgery.
Tendonitis: This term refers to an inflammation of a tendon - the fibrous tissue that connects a muscle to a bone. Tendons vary in shape and size and are responsible for moving the bones in the joints along with the muscles. Tendonitis is an extremely common condition often due to an overuse injury. Tendonitis causes pain near a joint and is worse with continued movement of that joint. Treatment options for tendonitis are aimed at reducing inflammation and include ice, rest, anti-inflammatory medications and cortisone injections.
Exercise-Induced Asthma: This condition is now known as exercise-induced bronchoconstriction (airway constriction or tightness). Symptoms of this bronchoconstriction include coughing, wheezing, chest tightness and shortness of breath brought on by exercise. These symptoms usually appear during exercise and continue to worsen for a while upon cessation of the exercise activity. Exercising in cooler, drier air is more likely to stimulate this reaction. The mainstay of treatment for this condition includes using short and long-acting bronchodilating (airway opening) inhalers prior to exercising.
Concussion: This term refers to a traumatic brain injury resulting from a blow to the head. Most concussions do not cause people to lose consciousness. Symptoms of a concussion include headache, confusion, dizziness, memory loss, ringing in the ears, nausea/vomiting, visual disturbances, and sensitivity to light. Although mild concussions are not usually life-threatening, they still should be evaluated by a medical professional to ensure there is no risk of permanent damage. For more severe concussions, a hospital admission for observation or appropriate imaging studies such as an MRI or CT scan may be warranted.
Heat Illness: A heat illness (also known as a heat stroke) is a common risk for those participating in sports or exercise activities in the summer months. Heat stroke is especially common for football players and runners, and is caused by a combination dehydration, not being acclimated to the heat, extreme heat and humidity, and body mass composition. Early signs of heat stroke may include irritability or confusion, vomiting, and chills. Later signs of heat stroke include hyperventilation (fast breathing), loss of balance while walking and seizures. Treatment of heat stroke is aimed at cooling off the person with constant monitoring of their body temperature as well as hydration.
Eating Disorder: There are many types of eating disorders including anorexia nervosa and bulimia nervosa. In anorexia, those affected are thin and fearful of gaining weight, whereas those with bulimia usually eat too much and then purge their food afterwards to avoid gaining weight. Anyone can develop an eating disorder, but those with concomitant anxiety or depression are most commonly affected. Sudden weight loss, fatigue or vertigo, stomach pains and diarrhea or constipation, irregular heartbeats, irregular menstrual periods and reduced concentration are hallmark signs of an eating disorder. Eating disorders are prevalent in athletes of both sexes, and therefore prevention and screening programs are vital to ensure safety.
Ultimately, Sports Medicine Physicians help people recover from musculoskeletal injuries, improve their overall athletic performance, and learn better ways to prevent future injury.
Important physical activity guidelines recommended by the American College of Sports Medicine and advocated by the U.S. Department of Health and Human Services (HHS) include:
Finding the right Sports Medicine Physician is an important first step to get the right treatment. Sports Medicine specialists may be found within the fields of Internal Medicine, Family Medicine, Pediatrics, or in Physical Medicine and Rehabilitation. Although these primary care physicians subspecialize in sports-related injuries, they are often sought for their expertise in improving overall health and nutrition, and helping patients maintain strength and endurance for a more active lifestyle.
You can read more about Sports Medicine in the following links:
https://www.acsm.org
https://www.amssm.org
https://us.sagepub.com/en-us/nam/the-american-journal-of-sports-medicine/journa