

A Colorectal Surgeon is a Board-Certified Doctor who treats and diagnoses conditions related to the small and large intestines as well as the anus and rectal region. These surgeons have expertise in not only general surgery, but have also undergone advanced training in the medical and surgical management of diseases of the intestinal tract, colon, and rectum/anus and perianal area. Surgeons within this specialty have training in open abdominal surgeries as well as in minimally invasive procedures such as endoscopy or laparoscopy.
Typically, your Primary Doctor (Internal Medicine, Family Medicine) or your Gastroenterologist will refer you to the Colorectal Surgeon for evaluation of a specific condition or treatment of a given diagnosis. You can also learn about your colorectal surgeon by viewing his profile in myDoqter, and learning about his training, credentials as well as his expertise.
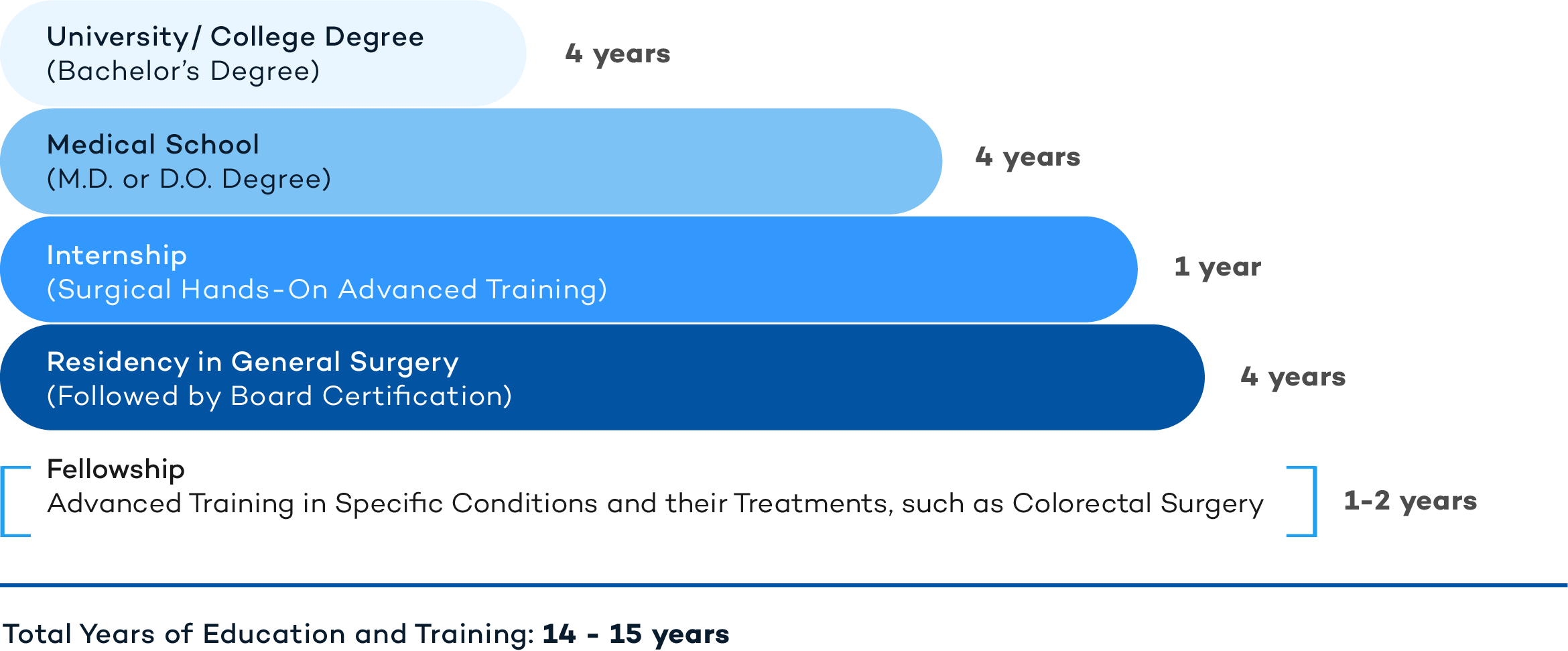
Colorectal Surgeons are doctors (M.D. or D.O.) with advanced medical degrees and training. The following is a representation of the years of education and training that a Colorectal Surgeon has undergone.
PROCTO from the Greek word ‘proktos’ meaning rectum, + LOGY from the Greek word ‘logia’ which means ‘logic’ or ‘the study of’.
A Colorectal Surgeon will treat an extensive list of conditions associated with the colon, anus and rectum, including:
Colon and Rectal Polyps: These growths occur on the lining of the colon and are generally considered benign. Although polyps are usually asymptomatic, some may be associated with rectal bleeding, changes in stool or bowel habits, or abdominal pain. Almost all cases of colon cancer, however, originate within polyps; therefore, regular screening exams after the age of 50 with colonoscopy should be performed to allow for their prompt detection and removal. Certain risk factors raise your risk of developing colon polyps including advanced age, obesity, family history of polyps, inflammatory bowel disease, excessive tobacco and alcohol use, and uncontrolled Type 2 diabetes.
Colon/Rectal Cancer: Colon/Rectal cancer refers to any cancer of the large intestine or rectum. Colon cancer may be completely asymptomatic in its earliest stages so regular screening exams (colonoscopy) are essential for early diagnosis. In later stages of colon cancer, patients may experience weakness or unexplained weight loss, abdominal discomfort, rectal bleeding or other changes in stool or bowel habits. Risk factors for colon cancer include advanced age, African American race, inflammatory bowel conditions, personal history of colon polyps, family history of colon cancer or genetic syndromes that include colon cancer risks, diabetes, obesity, smoking, excessive alcohol use and low fiber, high fat diets. Treatment of colon cancer depends upon the size, stage and location of the underlying cancer. Surgical resection of the affected portion of the colon with or without the rectum is the most common treatment for colon cancer. Chemotherapy may be needed to help shrink the tumor before surgery, or may be used with radiation following surgery to reduce the chances of a cancer recurrence.
Inflammatory Bowel Disease (IBD): This is a general term to describe inflammation of the gastrointestinal tract that may lead to damage of the tissue over time. The two most common forms of IBD include Crohn’s Disease and Ulcerative Colitis. Crohn’s Disease most commonly affects the small intestine but it can affect any part of the gastrointestinal tract. Ulcerative colitis, by contrast, only occurs in the large intestine and rectum. Symptoms of IBD include weight loss, fatigue, chronic and persistent diarrhea, abdominal pain and rectal bleeding. IBD is considered a dysfunction of the immune system and may also have a genetic predisposition leading to its development. IBD is usually diagnosed with upper endoscopy for Crohn’s Disease and via colonoscopy for Ulcerative Colitis. Treatment options are vast for IBD and include oral corticosteroids, immunomodulators, and the newer class of biologic agents. Crohn’s and Ulcerative Colitis represent very serious bowel conditions that may predispose patients to colon cancer, skin and joint inflammation, blood clots, as well as lead to malnutrition, bowel obstructions, ulcers and fissures without successful treatment.
Diverticulitis: This condition refers to inflammation or infection of pouches (diverticulae) that form in the wall of the intestines. Diverticulae may be painless and go unnoticed or they may be associated with abdominal pain, nausea and vomiting, fever and constipation. Mild diverticulitis may be treated with rest or antibiotics, but more severe or recurring bouts of diverticulitis may require surgical resection of the affected area.
Anal Fissures: These fissures are tears in the mucosal lining of the anus. These cracks and tears may cause pain and bleeding during bowel movements. Passing large or hard stools may produce these fissures. Eating foods high in fiber and ensuring proper hydration and avoiding straining during bowel movements usually helps to avoid this condition.
Incontinence: This is the loss of bowel control with leakage of fecal contents from the rectum. Damage to the muscle around the anus is the most common cause of incontinence (usually from a vaginal birth affecting the muscles or nerves of the anus). Other causes of incontinence include inflammatory bowel disease, diarrhea, stool impaction, nerve damage or from radiation treatment to the rectum.
Constipation: This is when a person has difficulty with bowel movements or has less than 3 bowel movements a week. It may be caused by dehydration, inactivity or lack of exercise and due to side effects from certain medications. Constipation is a common complaint to the colorectal surgeon, but sometimes it may reflect a serious underlying condition and therefore should be investigated with medical testing and treated appropriately so as to avoid a possible surgical intervention.
Rectal Prolapse: A rectal prolapse occurs when a portion of the large intestine or rectum lose their normal internal attachments and slip outside the anal opening. Rectal prolapse occurs in older adults, with women having a much higher overall incidence than men. A long-standing history of diarrhea or constipation with straining may predispose patients to this condition. Surgical repair is the mainstay of treatment for this condition and it usually has a high success rate.
Ultimately, Prevention with adequate screenings and a healthy, fiber-rich diet, are the most important steps towards maintaining the health of your colon. The American Society of Colon and Rectal Surgeons recommend that colorectal health be emphasized, especially in those over age 50, including regular colon screenings and removal of polyps before they become cancerous. Colon cancer is, unfortunately, common with approximately 140,000 new cases diagnosed each year. Colon cancer is largely preventable and making certain lifestyle choices can ensure good long-term colon health.
Important lifestyle measures to avoid colon cancer and other abnormalities of the gastrointestinal tract include:
Finding the right physician is an important first step to get the right treatment. Colorectal surgeons are trained to offer a wide range of treatment options that are tailored to your specific condition. Personalized plans will help you to manage your illness in the most effective manner.
You can read more about Colon and Rectal Surgery in the following links:
https://fascrs.org
https://www.ama-assn.org/specialty/colon
https://www.crohnscolitisfoundation.org
https://www.ccalliance.org